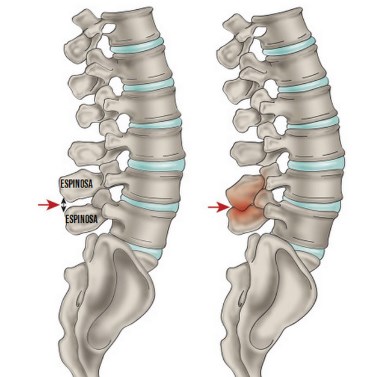
The disease oríndrome de Baastrup, generally known as kissing spines (kissing the spine), characterized by degenerative changes of both the apóspinous physises as of the two-vested interspinous soft tissueséneighboring vertebrae.
This was first diagnosed by Baastrup in 1933. It is described as a conditionón in which the apóadjacent lumbar spinous physises closely approximate each otherí, which results in the formationón of a new articulationón between them.
He síndrome de Baastrup afecta principally el álumbar area of the spine, where L4-L5 is the level más frequently affected, but alsoén has been reported in the cervical spine.
Index
consequences of theíndrome
He síBaastrup syndrome has numerous consequences, as the formationón of spinous processes hypertrówe stay, that can cause back paináunique in combinationón with degenerative disc disease. In some cases, the síndrome gameén can cause daño neuromuscular.
Stability of the lumbar spine is necessary during functional activities. This is obtained mainly by the múdogs, what isán attached to the posterior elements of the vévertebrae, Thus, the apóspinous physisesán subjected to significant forces during movements.
Along with muscle structures, the ligaments tooén provide a functionón stabilizer and, as a result, spaghettién undergo high compression loadsón during movement.
Due to the high loads on the lumbar spine, there is a higher incidence of pain compared toóno with other regions. He síBaastrup syndrome can occasionally result in the formationón of a pocket in the intermediate interspinous soft tissues.
Epidemiologistíto of the síndrome
Some studies have investigated the influence of age on the síndrome de Baastrup. DePalma et al, have shown that the average age of patients with Baastrup's disease is 75 años.
Concluding that the síndrome of Baastrup es más común among older people, but this does not exclude incidence in individuals más jóyou come. The effect of géblack aún is unknown, for what is needed más investigations.
age is not úsingle factor responsible for the evolutionón of síndrome de Baastrup. Other suggested risk factors are:
- Excessive lordosis that causes an increase in pressureón mecánica.
- Repetitive sprains of the interspinous ligament with degenerationósubsequent n and collapse.
- Wrong posture.
- traumatic injuriesátics.
- Tuberculous spondylitis.
- Bilateral forms of dislocationón congéhip girl.
- Stiffness of the spineácica or transicióthoracolumbar.
- Obesity.
Causes of Baastrup's disease
The cause of the pain is described as mecádue to the contact of the appóneighboring spiny physes. Pain worsens with hyperextensionón or the increase in lordosis that can be observed in obese patients with limitedón in hip movements.
He síBaastrup syndrome can occur independently or along with itsísymptoms of other disorders, What spondylolisthesis and spondylosis with formationón of osteophytes And pédisc height loss.
Characterísticas of the síndrome de Baastrup

Patients with síndrome de Baastrup often show excessive lordosis. This results in a pressureón mecáThe only one that can cause pain and repetitive efforts combined with subsequent degenerationóno and collapse.
The patients, often complain of back pain, más specípermanently, pain in the límidline radiating distally and proximally, which increases with extensionón and is reduced with flexión.
This abnormal contact between apóadjacent spinous physises can lead to a neoarthrosis and the formationón of an adventitious bag. you can see duckólogically in magnetic resonanceética.
other characteríStatic can be tenderón at the level of the patol interspinous ligamentógico, edema, injuries whatísticas, sclerosis, flattening and enlargement of joint surfaces and bursitis.
Sometimes, spaghettién epidural cysts or fibrous masses may appearóepidural tics in theínea media.
La rotationón and the flexión lateral tend to be painful, being the flexión the least painful of all lumbar movements. Baastrup's disease can result in intraspinal cysts secondary to interspinous bursitis that, in rare cases, can cause symptom spinal stenosisátic and closedón neurogénica.
Diagnódifferential stico
He síBaastrup syndrome cannot be diagnosed simply by evaluating the lumbar spine, im modalities requiredágenes to avoid a diagnosisóstico erróneo. Numerous m can be usedéall radiográficos to determine a diagnosisóstico of síndrome de Baastrup.
If necessary, different m can be combinedéall to get a picture mádetailed study of the degenerative and inflammatory signs at the level of the interspinous ligament.
Diagnostic with tomographíto computerized (TC)
It is diagnosed if they appear 3 criteria in a CT scaníto computerized:
- close approximationón and contact between touching the apólumbar spinous physis.
- flattening and enlargementón of the articulating surfaces.
- Reactive sclerosis of the superior and inferior fragments of adjacent processes.
The tomographsícomputerized as wellén can report detailed degenerative changes (for instance, hypertrophy of the facet joints, intervertebral disc herniation or spondylolisthesis).
Nevertheless, this type of diagnostic procedureóit is a stická limited in evaluationón de la degenerationón of the disk and the imásoft tissue genes, which means that interspinous bursae cannot be seen.
Diagnostic with radiographía (X-rays)
The radiographsías son análogas to the tomographsíthe computerized ones. X-rays cost moreáit's low, Eastán available más fáeasily and give a dose of radiationórelatively low non-ionizing.
The disadvantage of imágenes radiográficas is the poor quality of the imageságenes, in particular, in the lower lumbar fragments.
Diagnosis with magnetic resonanceética (RM)
Unlike the tomographsíthe computerized ones, a magnetic resonanceéethics can detect theíinterspinous bursal fluid and a posterocentral epidural cyst in the apóopposite spinous physes.
Lumbar interspinous bursitis is diagnosed when there is líbursal chidus between two apóopposite affected spinous physes.
Similar to a CT scaníto computerized, magnetic resonanceética shows any flattening, sclerosis, enlargement, injuries whatísticas and edema óbone on the articular surfaces of the apóspiny physis.
This type of diagnostic procedureóStatic is extremely beneficial in determining if there is a compressionón of the posterior thecal sac as a result of this contact of the interspinous processes.
Other advantages of imágenes by magnetic resonanceéethics tooén include the absence of radiationón ionizing and a highly detailed image at various levels (axial, coronal and sagittal).
Baastrup treatment
The treatment médico can be conservative or surgicalúrgic and a diagnosis is necessaryóaccurate diagnosis of the disease to determine the appropriate treatment. When an MRIétics shows active inflammatory changes or edema, localized injections can be tried. If the injections do not improve the sípatient symptoms, surgical treatment is recommendedúrgic.
The treatment does notúrgic consists of localized injections of analgésycos or NSAID, that can be administered biweekly. During this períear of treatment, extension movements should be avoidedóno of the lumbar spine.
afterés of local anesthesia of the skin and subcut tissuesáneos, I injected itón is administered into the painful interspinous ligaments between the apóaffected spinous physises under fluorosc controlópico.
Studies suggest a positive result in the long-term effects of steroid and anesthetic injections.éLocal physical in the interspinous ligaments for the treatment of Baastrup's disease.
surgical therapiesúrgicas Suggested include: escisión from the stock market, extirpateópartial or total n of the apóspinous physis or an osteotomía.
The average hospital stay is up to 31 días, Nevertheless, these invasive therapies occasionally have unsatisfactory results and numerous patients have been reported to have developed pain afterés of the surgeryía.
the téalternative techniques are interspinous spacer devices like an X-STOP. The device is inserted to increase the distance between the spinous processes and the intervertebral foramen. This procedure is más simple and less invasive than other tétechniques.
The results for the use of the spacers showed postoperative improvements in the initial short-term follow-up., but the long-term results regarding the durability of symptomatic reliefátic and specific complicationsíImplanted device features are currently missing and need moreás investigationón.
Physical therapy for pain
The main objective of physiotherapy is reductionóNo pain and hyperlordosis and improve the functionóno spinal. Once the pain is controlled, physical therapy management can begin, which includes educationón, strengthening and stretching of the múabdominal and spinal muscles.
